Choosing a fixed solution for missing or failing teeth is rarely a simple decision. Patients considering full-arch dental implants are often balancing comfort, durability, cost, recovery time, and long-term maintenance. Two approaches dominate modern full-arch rehabilitation: the traditional four-implant protocol and expanded designs that use additional implants when clinical conditions demand it.
Rather than framing this choice as a competition, this article examines how these protocols differ in biomechanics, clinical outcomes, technology, and patient suitability. The goal is not to sell a single approach, but to clarify why one method may be more appropriate than another depending on anatomy, bite force, material choice, and long-term risk management.

What Is the All-on-4 Dental Implant Concept?
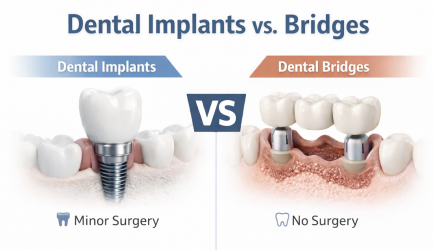
The All-on-4 dental implant is a full-arch implant approach designed to support a fixed prosthesis using four strategically placed implants. Two implants are typically placed in the front of the jaw, where bone density is often higher, while two posterior implants are angled to engage available bone and avoid anatomical structures such as the maxillary sinus or the inferior alveolar nerve.
This configuration allows a fixed prosthesis to be supported without placing an implant for every missing tooth. The prosthesis is commonly a fixed hybrid denture, meaning it replaces both teeth and missing gum tissue in a single unit. In suitable cases, a temporary fixed bridge may be attached shortly after surgery through immediate loading, allowing patients to leave without a removable denture.
Immediate loading does not eliminate healing. Osseointegration still occurs over several months, and the temporary bridge is designed to protect implants while tissues adapt. The final prosthesis is fabricated only after stability and soft-tissue health are confirmed.
How All-on-X Differs From a Strict Four-Implant Protocol
Expanded full-arch designs, often referred to as All-on-X, allow clinicians to adjust implant number and placement based on patient-specific factors. Instead of limiting treatment to four implants, additional implants may be placed to improve load distribution, reduce cantilever length, or compensate for softer bone.
The presence of more implants does not automatically improve outcomes. Extra implants are beneficial only when they solve a biomechanical or anatomical problem. In cases with heavy bite forces, long arch spans, or planned zirconia prostheses, additional support points can reduce mechanical stress on individual implants and prosthetic components.
In patients with strong bone quality, controlled occlusion, and excellent hygiene access, four implants may provide predictable and durable results without unnecessary complexity.
Why Function and Maintenance Matter More Than Implant Count
Most patients pursue fixed full-arch solutions to restore comfort, confidence, and function. Improved chewing efficiency, clearer speech, and elimination of denture movement are common goals. Facial support is another consideration, as long-term tooth loss can alter lower facial height and appearance.
What is often overlooked is maintenance. A fixed bridge is not a “set it and forget it” solution. Daily cleaning under the prosthesis is essential, and professional maintenance visits are required to monitor tissue health, prosthetic wear, and bite balance. Designs that limit cleaning access may appear attractive initially but increase long-term risk.
Understanding how implants fit within broader treatment planning is important. Many patients compare fixed full-arch options with alternatives such as implant-supported dentures or snap-in systems, each with distinct advantages and maintenance demands.
For an overview of implant options beyond full-arch rehabilitation, the dental implants service page provides additional context:
Clinical Success Rates and Long-Term Outcomes
When patients ask about success rates, they usually mean two things: implant survival and prosthesis survival. Long-term studies and systematic reviews consistently report high survival rates for full-arch implant systems when cases are well planned and maintained.
A 2023 review of the All-on-4 concept reported favorable long-term outcomes and noted that immediate and delayed loading protocols can both perform well in properly selected cases. Reported 10-year survival rates ranged from approximately 93% to 95% depending on loading strategy and study design.
A landmark longitudinal cohort by Maló and colleagues reported prosthesis survival exceeding 99% over up to 10 years in full-arch mandibular cases. These figures do not imply an absence of complications. Instead, they demonstrate that with risk management and maintenance, full-arch systems can remain functional for many years.
Comparisons between four-implant and six-implant designs often show similar survival rates. Differences tend to be linked to biomechanics, bone quality, and patient habits rather than implant number alone.
How does All-on-X differ from traditional All-on-4?
Because medical and dental regulations limit precise pricing in educational content, relative comparisons are more appropriate than fixed numbers.
| Feature | All-on-4 (typically 4 implants) | All-on-X (5–8 implants) |
|---|---|---|
| Surgical complexity | Moderate | Higher |
| Material durability | Good (acrylic commonly used) | Excellent (zirconia more frequent) |
| Aesthetics | Good | Superior |
| Long-term repair likelihood | Higher | Lower |
| Upfront investment | Lower | Higher |
| Suitability for weak bone | Limited | Very good |
| Force distribution | Moderate | Improved (shorter cantilevers possible) |
| Mechanical redundancy | Low | High |
| Ideal patient profile | Moderate bone, lower bite force | Severe atrophy, bruxism, longevity-focused |
These comparisons reflect relative clinical complexity, not exact cost. Treatment plans should always include a written scope of work outlining implants, materials, temporary prosthesis, sedation, maintenance expectations, and warranty terms.
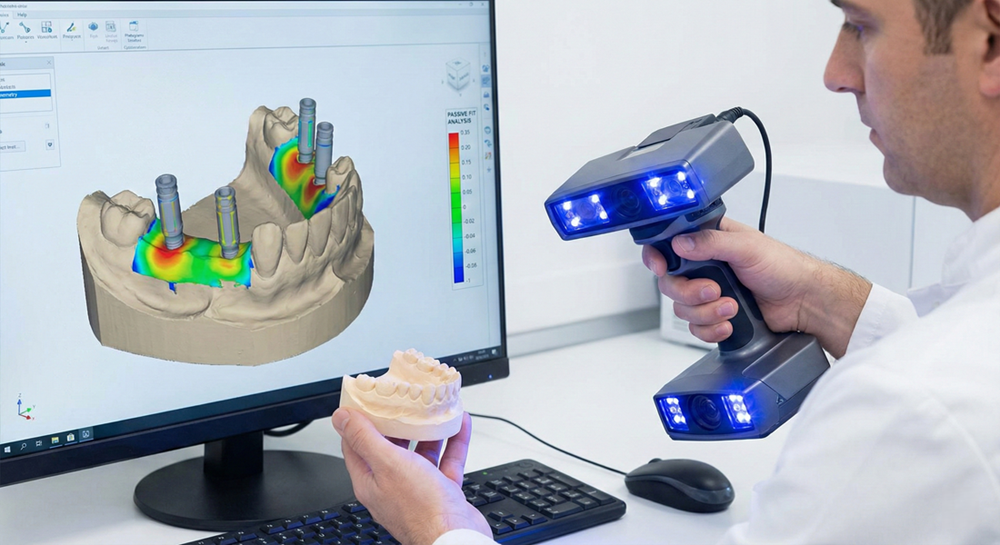
Digital Planning and Technology Advancements by 2026
By 2026, digital workflows dominate full-arch implant planning. Cone-beam CT imaging, intraoral scanning, and guided surgery allow implants to be placed based on prosthetic goals rather than bone availability alone.
One of the most significant advances is photogrammetry, using systems such as PIC Dental or iMetric. These camera-based technologies capture implant positions with micron-level accuracy, eliminating distortion from traditional impressions.
The result is a passive-fit prosthesis that seats without internal stress. Passive fit reduces screw loosening, framework distortion, and long-term mechanical complications. For patients, this often translates to improved comfort and fewer adjustments over time.
How Tilted Implants Improve Stability: A Simple Explanation
Imagine pitching a tent. If tent pegs are driven straight into loose soil, the structure shifts. When pegs are angled outward, stability improves.
Tilted posterior implants work the same way. By angling implants into denser bone, clinicians avoid sinus cavities and reduce cantilever length. Shorter cantilevers decrease bending forces on implants and prosthetic screws, improving long-term stability.
A 2025 biomechanical study confirmed that framework material and cantilever length significantly influence stress distribution in full-arch restorations, reinforcing the importance of design over implant count alone.
How Many Implants Are Ideal in 2026?
Modern planning begins with the prosthetic outcome rather than implant number. The final tooth position, bite relationship, and hygiene access determine where implants should be placed.
Four implants may be ideal when stability is high and cantilevers are controlled. Six implants can reduce load per implant and provide redundancy. Additional implants increase surgical complexity and maintenance demands and should be justified by clinical need rather than routine preference.
Which patients benefit most from expanded designs?
Which Option Is More Appropriate for You?
This section helps clarify which full-arch approach may be more appropriate based on anatomy, bite force, and long-term priorities. Final decisions should always be made after clinical examination and imaging.
Profile A – All-on-4 is often suitable
- Adequate bone volume in key support areas
- No history of heavy bruxism or clenching
- Moderate bite force and shorter arch span
- Budget sensitivity is an important factor
- Comfortable with slightly higher long-term maintenance risk
Profile B – Expanded designs (All-on-X) are usually the better choice
- Softer bone quality, particularly in the upper jaw
- Advanced maxillary atrophy or long arch spans
- Heavy bite force or nighttime grinding habits
- Planned zirconia prostheses requiring higher rigidity
- Priority is long-term durability and minimal future repairs
- Willing to invest more upfront for improved force distribution
All-on-6 Dental Implants
Six-implant full-arch designs are commonly used when additional posterior support is needed to improve force distribution and reduce cantilever length. This option is often considered for patients with stronger bite forces, longer arch spans, or softer bone where extra stability reduces mechanical risk.
All-on-8 Dental Implants
Eight-implant configurations are less common and typically reserved for select cases with excellent bone volume and very high functional demands. The goal is maximum redundancy and load sharing rather than routine use, and this approach is not necessary for most full-arch patients.
Mini Case Study: Why One Patient Needed More Support
Real Patient Scenario (Composite Case)
John, a 58-year-old patient, presented with failing maxillary teeth, a history of heavy clenching, and relatively soft bone in the upper jaw. Although a four-implant configuration was technically feasible, biomechanical analysis showed elevated stress concentration due to his bite force and arch length.
To reduce mechanical overload and shorten cantilever length, the clinician recommended a six-implant design. The additional implants provided redundancy and improved force distribution. Two years after delivery of the final prosthesis, the restoration remains stable with healthy tissues and no mechanical complications.
This scenario illustrates why expanded designs are often chosen for risk reduction rather than marketing preference.
Common Complications and How They Develop
Complications fall into two categories: biologic and mechanical.
Biologic issues include peri-implant mucositis, peri-implantitis, and early implant failure. Mechanical issues include screw loosening, acrylic tooth fracture, ceramic chipping, and framework wear.
Risk factors include smoking, uncontrolled diabetes, heavy grinding, long cantilevers, and inadequate cleaning access. A useful patient test is simple: if the plan does not clearly show how the bridge will be cleaned, it is incomplete.
Materials and Prosthetic Design Choices
Material selection influences durability and maintenance. Acrylic-based bridges absorb shock and are easier to repair but wear faster. Zirconia offers superior strength and stain resistance but requires precise bite planning.
By 2026, full-arch treatment is shifting toward monolithic zirconia bridges and AI-assisted planning tools. These systems help optimize implant positioning, angulation, and load distribution. Early clinical data is also evaluating immediate loading of zirconia frameworks, though strict case selection remains essential.
Patients comparing fixed hybrid dentures, implant-supported dentures, and snap-in systems should consider long-term maintenance as carefully as initial comfort.

Patients comparing fixed options often review fixed hybrid dentures alongside removable alternatives.
Longevity and Expected Lifespan
Full-arch implant systems can last many years when maintained properly. A 2024 systematic review on immediate loading reported survival rates above 93% across included studies.
Longevity depends on patient behavior as much as surgical technique. Smoking, uncontrolled inflammation, and grinding increase risk. Routine maintenance and protective appliances such as night guards play a critical role.
Signs a Full-Arch Restoration Needs Attention
Warning signs include clicking, rocking, speech changes, persistent sore spots, bleeding, swelling, or bad taste. Early evaluation can prevent minor issues from becoming major repairs.
Future Trends: Zygomatic and Pterygoid Implants
For patients with severe maxillary bone loss, zygomatic and pterygoid implants offer alternatives to extensive grafting. These advanced techniques anchor implants in dense craniofacial bone and expand treatment possibilities for complex cases.
They are not first-line solutions and require specialized training and careful risk discussion, but their use is increasing as experience and technology advance.
Step-by-Step: What to Expect
- Consultation and records: Medical history, imaging, and bite evaluation
- Planning: Prosthetic-driven implant positioning, often with guided surgery
- Surgery day: Extractions if needed, implant placement, abutment connection
- Temporary bridge: Fixed or removable depending on stability
- Healing phase: Integration and tissue maturation
- Final prosthesis: Delivered once stability is confirmed
Self-Assessment Checklist
Profile A
- Adequate bone volume
- No heavy grinding
- Budget sensitivity
Profile B
- Softer bone or sinus anatomy challenges
- Heavy bite force
- Preference for maximum strength and longevity
What this article does NOT cover
This article focuses on clinical planning and long-term outcomes. It does not replace an in-person exam, imaging, or individualized treatment planning, which are essential for final decisions.
Final Thoughts
Choosing between full-arch implant protocols is not about winning a comparison. The best plan aligns anatomy, biomechanics, material choice, and long-term maintenance. When these factors are respected, full-arch implants can provide stable, comfortable function for years to come.
This article reflects current planning workflows and technologies commonly used in full-arch implant cases in 2026.