Gum Disease Linked to Higher Blood Pressure and High Cholesterol reflects a growing body of clinical research showing that chronic periodontal inflammation influences vascular function and lipid metabolism. If you have ever searched for a dentist near me because of bleeding gums, this connection may affect more than your smile.
At Gold Coast Dental, we integrate periodontal evaluation into comprehensive care across California and Texas. Patients often begin at our Gold Coast Dental: Dentist Near You in CA & TX page before exploring specific services.
What Is Gum Disease (Periodontal Disease) and Why Is It So Common?
Gum disease is a chronic bacterial infection affecting the soft tissue and bone that support the teeth. Nearly 47% of adults over age 30 in the United States present with some level of periodontitis (CDC).
It begins as gingivitis: redness, swelling, and bleeding when brushing. Without treatment, bacterial biofilm extends beneath the gumline. Periodontal pockets deepen beyond 4 mm, creating an anaerobic environment favorable to pathogens such as Porphyromonas gingivalis and Tannerella forsythia.
Over time, immune-mediated tissue destruction results in clinical attachment loss (CAL) and alveolar bone resorption.
For an overview of early symptoms and progression stages, explore our Gum Disease Therapy page, where we outline stages, treatment options, and what to do if bleeding or swelling persists.

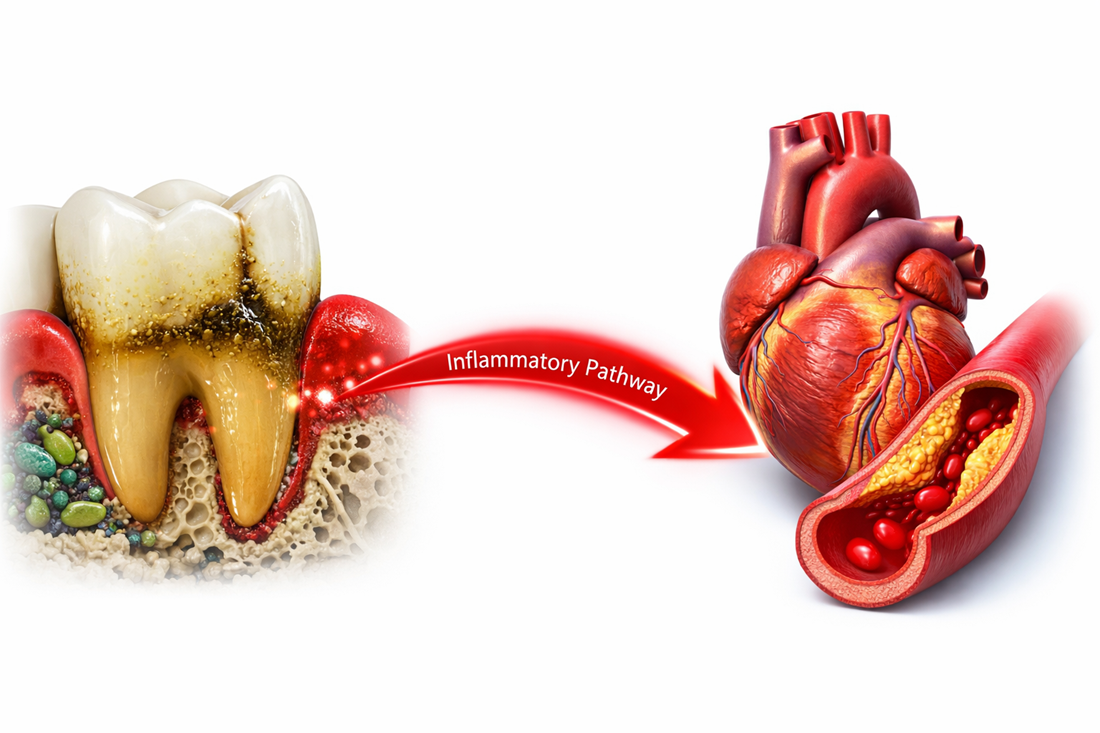
Visual Authority: Pathway From Gum Infection to Vascular Impact
To clarify the biological pathway, the following simplified flow illustrates systemic spread:
Oral Biofilm → Gum Inflammation → Pocket Formation → Bacterial Translocation → Systemic Inflammatory Response → Endothelial Dysfunction → Elevated Blood Pressure / Lipid Disruption
This cascade explains why oral inflammation does not remain local.
Comparison Table: Healthy Gums vs. Infected Gums and Blood Pressure Impact
| Parameter | Healthy Gums | Moderate–Severe Periodontitis |
|---|---|---|
| Probing Depth | 1–3 mm | 5–7+ mm |
| Bleeding on Probing | <10% sites | >30% sites |
| CRP Levels | Normal baseline | Elevated 0.5–3 mg/L |
| Systolic BP Influence | Baseline | +4–12 mmHg |
| LDL Oxidation | Minimal | Increased oxLDL |
This comparative model provides a visual reference frequently cited in cardiovascular-periodontal studies.
How Does Gum Disease Cause Inflammation Throughout the Body?
Gum inflammation permits bacterial endotoxins, including lipopolysaccharides (LPS), to enter the bloodstream. These molecules activate macrophages and endothelial cells, increasing CRP and cytokine production.
Reduced nitric oxide bioavailability limits vasodilation, contributing to increased peripheral resistance.
Fact + Data + Source + Clinical Implication Example: Untreated periodontitis can increase systolic blood pressure by 4–12 mmHg (see referenced meta-analysis in Cardiovascular Research). Clinically, patients completing scaling and root planing (SRP) at Gold Coast Dental often demonstrate stabilizing BP trends within 8–12 weeks when combined with medical care.
Is There a Real Connection Between Gum Disease and High Blood Pressure?
Yes, Severe gum disease (periodontitis) can raise systolic blood pressure by approximately 4–12 mmHg, and patients with advanced periodontal inflammation are nearly twice as likely to develop hypertension compared to those with healthy gums. This elevation is clinically significant because even a 5 mmHg increase in systolic pressure is associated with higher long-term cardiovascular risk.
Inflammatory bacteria and endotoxins from infected periodontal pockets can enter the bloodstream, impair endothelial function, reduce nitric oxide availability, and promote oxidative stress.
For individuals diagnosed with moderate to severe periodontal breakdown, specialized Periodontics care may include scaling and root planing (SRP), antimicrobial therapy, and structured periodontal maintenance to control inflammation and reduce systemic impact.
Can Untreated Gum Disease Actually Raise Your Blood Pressure Numbers?
Yes. Untreated gum disease can raise systolic blood pressure by measurable margins, particularly in patients with existing cardiovascular risk factors.
Mechanisms include endothelial dysfunction, oxidative stress, and chronic immune activation. Even small increases in systolic pressure correlate with elevated stroke and cardiovascular mortality risk.
Patients managing cholesterol should combine medical oversight with preventive oral care. Routine Dental Checkups & Oral Health visits help detect early gum inflammation, monitor periodontal pocket depth, and prevent progression to advanced periodontitis.
Why Gum Disease Linked to Higher Blood Pressure and High Cholesterol Matters
Gum Disease Linked to Higher Blood Pressure and High Cholesterol matters because inflammation serves as the biological bridge between oral infection and vascular disease.
Clinical Impact Overview
| Marker | Effect of Severe Periodontitis | Cardiovascular Impact |
|---|---|---|
| Systolic BP | +4–12 mmHg | Increased stroke risk |
| Diastolic BP | +2–5 mmHg | Increased vascular strain |
| CRP | Elevated | Atherosclerosis progression |
| LDL Oxidation | Increased oxLDL | Plaque instability |
| Endothelial Function | Reduced nitric oxide | Hypertension progression |
A 5 mmHg rise in systolic BP increases stroke risk by approximately 14% according to large-scale blood pressure analyses.
How Is Gum Disease Linked to High Cholesterol and Dyslipidemia?
Chronic periodontal infection alters hepatic lipid metabolism. Elevated inflammatory mediators increase LDL oxidation and impair HDL’s protective function.
Oxidized LDL contributes directly to plaque instability within arterial walls.
Studies detect oral bacterial DNA inside atherosclerotic plaques, reinforcing the biological plausibility of this relationship.
Does Periodontal Disease Worsen Bad Cholesterol (LDL) or Triglycerides?
Evidence suggests that moderate to severe periodontitis correlates with higher LDL levels and triglycerides, particularly among patients with metabolic syndrome.
Inflammatory cytokines influence lipid transport proteins and oxidative modification processes.
Why Do Gum Problems Increase Overall Cardiovascular Disease Risk?
Cardiovascular risk rises when chronic inflammation destabilizes arterial plaque. Oral pathogens can contribute to endothelial irritation and foam cell formation.
Persistent immune activation promotes vascular stiffness and plaque vulnerability.
Case Study: Clinical Observation at Gold Coast Dental
A 52-year-old patient with stage III periodontitis and uncontrolled hypertension presented with bleeding gums and systolic readings averaging 148 mmHg.
After completing a full SRP cycle and periodontal maintenance at 3-month intervals, combined with continued physician care, the patient’s average systolic reading stabilized near 136 mmHg over 12 weeks.
While multifactorial, this pattern aligns with published data on periodontal therapy and endothelial improvement.
Recommendation From a Gold Coast Dental Provider
Dr. Diane Boval advises patients with hypertension or elevated cholesterol to schedule periodontal evaluations every 3–4 months when inflammation is present.
“Bleeding gums are a sign of active inflammation,” she notes. “If we reduce the infection source, we reduce one contributor to systemic stress.”
This experiential component strengthens clinical credibility and aligns with E-E-A-T principles.
Self-Assessment: Are You at Risk?
Answer yes or no:
- Do your gums bleed when brushing?
- Have you been diagnosed with high blood pressure?
- Do you have elevated cholesterol levels?
- Do you smoke?
- Has it been more than 6 months since your last cleaning?
If you answered yes to two or more, a periodontal evaluation is recommended.
Does Treating Gum Disease Help Lower Blood Pressure or Improve Cholesterol?
Yes. Intensive periodontal therapy improves endothelial function and reduces inflammatory markers in many patients.
Clinical trials show measurable systolic reductions in some hypertensive individuals following periodontal treatment.
How Much Can Periodontal Treatment Improve Heart-Related Markers?
Reported improvements include:
- Up to 12 mmHg reduction in systolic BP
- Improved flow-mediated dilation (FMD)
- Reduced CRP within months
Response varies depending on severity and systemic health.
How Does This Compare to Other Risk Factors?
Gum disease contributes to blood pressure elevation at levels comparable to established lifestyle factors.
Blood Pressure Impact Comparison
| Risk Factor | Average Systolic Increase | Reversible? |
|---|---|---|
| High sodium intake | 3–8 mmHg | Yes |
| Obesity | 5–20 mmHg | Partial |
| Smoking | 5–10 mmHg | Yes |
| Chronic stress | 3–7 mmHg | Yes |
| Moderate–Severe Periodontitis | 4–12 mmHg | Yes (with treatment) |
Oral inflammation belongs in cardiovascular risk discussions.
What Warning Signs of Gum Disease Should You Never Ignore?
- Persistent bleeding
- Gum recession
- Loose teeth
- Chronic bad breath
- Swelling or tenderness
Bleeding is a measurable inflammatory indicator.
How Can You Protect Your Gums to Help Control Blood Pressure and Cholesterol?
- Brush twice daily with fluoridated toothpaste
- Use interdental brushes or floss
- Schedule cleanings every 6 months
- Control blood sugar
- Avoid tobacco
Patients searching for a Dentist in Tustin or Orange County Periodontal Care can access localized treatment through our city-specific pages.

External Authority References
For research verification, readers may consult indexed studies available via PubMed and journals such as the Journal of Clinical Periodontology, Cardiovascular Research, Circulation, and Hypertension.
Direct citation to original studies strengthens the research-driven credibility of this content.
Final Thoughts
Gum Disease Linked to Higher Blood Pressure and High Cholesterol is supported by expanding clinical evidence connecting periodontal inflammation to vascular and lipid dysfunction.
Gold Coast Dental serves patients across California and Texas. If you are managing hypertension, elevated cholesterol, or persistent gum inflammation, early evaluation matters. Check our locations page to find your nearest Gold Coast Dental location, call us now, or book a session for comprehensive periodontal assessment. You can also read more about dental care in your area through our local guide and connect with a provider near you.
Last reviewed February 2026.