What Is Gum Disease?
Gum disease (periodontal disease) is an infection and inflammation of the gums and supporting bone. It often starts as gingivitis (reversible) and can progress to periodontitis, where bone and attachment are lost.
What causes it?
Plaque bacteria trigger the body’s response. Over time, plaque hardens into tartar, pockets deepen, and tissues break down. Smoking, diabetes, and inconsistent home care raise risk..
Early signs to watch
- Bleeding when brushing or flossing
- Puffy or tender gums
- Bad breath
- Gum recession or “longer” teeth
- Teeth that feel slightly loose or shifting
Why does gum disease matter for whole-body health?
Studies link periodontal disease with heart health and diabetes control. Therapy can modestly lower A1c in people with diabetes in the short term (about 0.3–0.4%).
Can gum disease kill you?
It isn’t usually fatal alone, but long-standing oral infection relates to higher systemic risks. Fast action and steady care protect you.
Can gum disease cause bad breath?
Yes. Most odor starts in the mouth—often from tongue coating and inflamed gums. Treating infection and cleaning the tongue help.
Gum disease treatment options for severe cases
Advanced sites may need periodontal surgery to access deep calculus, reshape bone, or attempt regeneration. Unsalvageable teeth can be replaced with implants or bridges.
Can gum disease be reversed?
Gingivitis: Yes—consistent daily care plus professional cleanings.Periodontitis: It’s manageable. With the right plan and maintenance, you can stop infection and protect function.
How do dentists treat gum disease?
Step 1 — Deep cleaning (scaling and root planing).
Removes plaque and tartar below the gumline. Typical pocket improvements are about 1–2+ mm, especially at deeper sites.
Step 2 — Supportive tools (as needed).
Local antibiotics, antimicrobial rinses, or laser-assisted therapy in select cases.
Step 3 — Re-check at 4–8 weeks.
We measure healing and decide next steps. Severe sites may need periodontal surgery or regeneration.
Need a visit? Start with a gentle cleaning and exam: book now or see services.
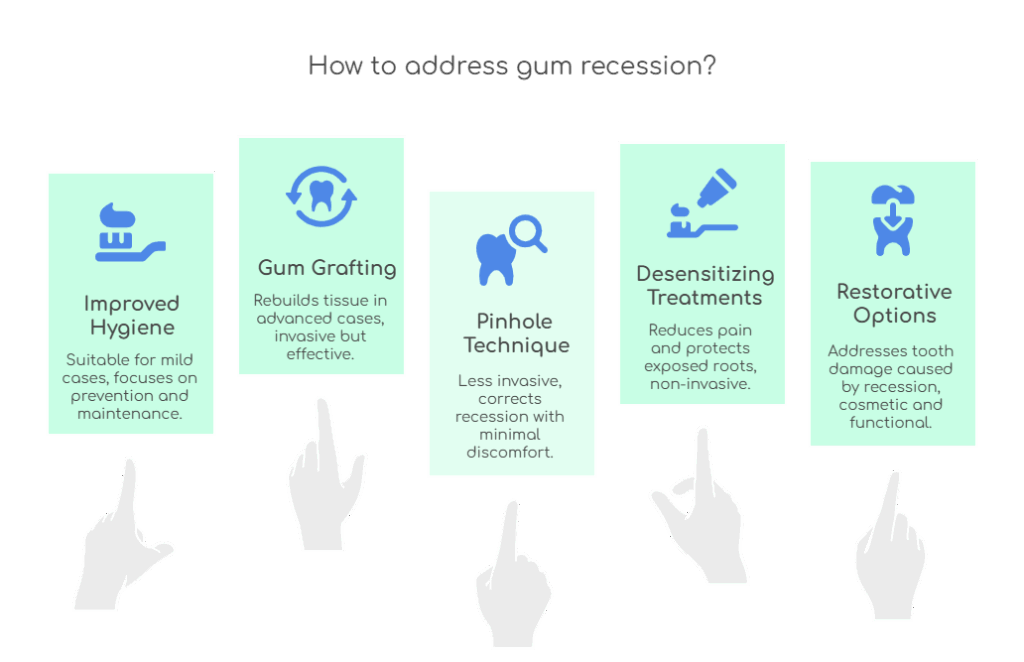
How to Get Rid of Gum Disease?
For early disease, consistent gum disease self-care plus professional cleanings often return gums to health. For advanced cases, Gum Disease Therapy plus maintenance every 3–4 months keeps it stable.
What can I do at home?
You can’t remove hardened tartar at home, but you can calm inflammation and protect your gums:
- Brush 2×/day for 2 minutes with a soft brush and fluoride toothpaste
- Clean between teeth daily (floss or interdental brushes)
- Add an antimicrobial rinse if your dentist suggests it
- Keep regular cleanings and checkups
- Limit added sugar; if you smoke, ask for support to quit
For braces or hard-to-reach areas, a water flosser can help you clean around brackets and under wires.
Pediatric Dentistry: Healthy Gums from the Start
Pediatric dentistry for gum disease prevention focuses on coaching kids and parents. Teens with braces need extra tools to avoid swollen gums around tooth brackets and plaque traps.Figure 1 — At-a-Glance Outcomes & Numbers
| Measure | Typical Result |
|---|---|
| U.S. adults 30+ with periodontitis | 42.2% |
| Global severe periodontal disease | >1 billion cases |
| A1c change after periodontal therapy (diabetes) | ~0.3%–0.4% ↓ (short term) |
| Probing depth reduction after non-surgical therapy | ~1–2+ mm |
| Halitosis of oral origin | ~80% |
How long does treatment take?
- Deep cleaning: Often one to two visits
- Re-check: 4–8 weeks after cleaning
- Maintenance: Every 3–4 months for periodontitis to keep pockets stable.
Costs and insurance
Scaling and root planing is billed per quadrant, and many plans cover part of it. Adjuncts and surgery vary by plan and diagnosis. We can check your benefits for you during your visit.
Myths vs. Facts
“No pain means no problem.” Early disease is often quiet; bleeding is a warning sign.“Mouthwash replaces floss.” Rinses help, but they don’t clean between teeth.“Bad breath is from the stomach.” Most odor starts in the mouth, especially with inflamed gums.
Prevention that works
- Brush 2×/day, clean between teeth daily, and book care on schedule
- Look for bleeding, persistent bad breath, or gum tenderness—these call for an exam
- Kids and teens: coaching plus the right tools helps prevent swelling around braces
How We Personalize Care
We stage disease by depth and attachment loss, then grade by risk and speed of change. This guides non‑surgical therapy, surgery, or combined plans to protect long‑term function.
Patients typically ask :
Bleeding, Natural Care, Timing, and Diet
Why do my gums bleed when I brush?
Most bleeding comes from inflamed tissue caused by plaque along the gumline. Switch to a soft brush, clean between teeth daily, and schedule a professional cleaning; if bleeding lasts more than a week, book an exam to rule out deeper pocketing or other causes.
Can I treat gum disease naturally?
Healthy habits help: twice‑daily brushing, interdental cleaning, and a balanced diet low in added sugar. Warm saltwater rinses may soothe minor irritation, but mineralized calculus needs professional removal; home remedies can’t replace deep cleaning for established periodontitis.
How long does gum disease treatment take?
Most deep cleanings are completed in one to two visits, followed by a 4–8 week check to measure healing. Maintenance visits every 3–4 months keep pockets stable; advanced cases may need additional appointments for surgical or regenerative care.
What foods help prevent gum disease?
Choose fiber‑rich fruits and vegetables, dairy or calcium‑fortified options, lean proteins, and plenty of water. Limit sticky sweets and acidic drinks that feed plaque and irritate tissues; vitamin C–rich snacks (such as citrus or berries) support collagen and healing.
Gum Disease is common—but manageable with a plan, steady home habits, and routine maintenance. If you want a clear path from a Dentist in California or a trusted team “near me” in Texas, we’re ready to help. Gold Coast Dental has 19+ locations across California and Texas; check our locations page to find your nearest Gold Coast Dental location. To get started, call us now or book a session, and visit our local guide to read more about dental care in your area.